As vaccines have become readily available to people age 16 and up, Dr. Justin Pruneski, an associate professor and chair in the department of Biological and Environmental Sciences, covered a discussion on COVID-19 and vaccine questions and concerns. This discussion was open to all students and faculty on Thursday, April 21, and was followed by a live Q&A.
Understanding the immune system was the first topic covered. “Within the human immune system, there are antibodies which can target specific pathogens and respond to it in order to clear it out and render it less dangerous to our health,” explained Dr. Pruneski. Antibodies result from the body recognizing a pathogen and then forming a response to it that can then remember that specific pathogen. If/when the body comes in contact with that pathogen again, it can then recall it and fight it off much faster and stronger.
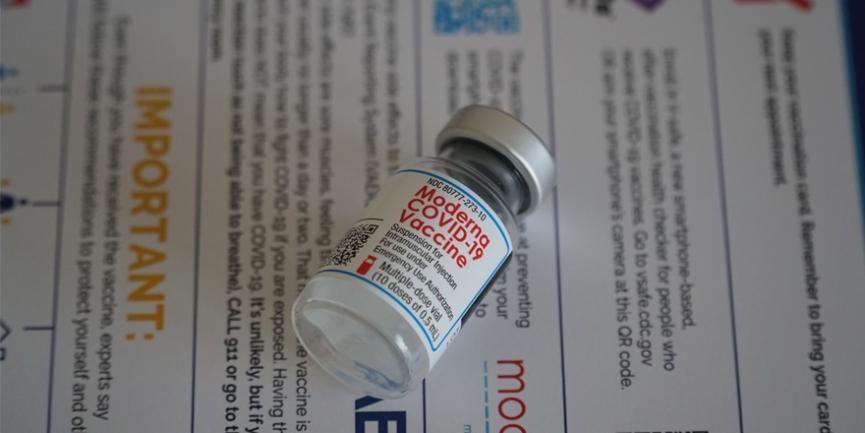
“Vaccines are a different tactic of fighting off pathogens,” Dr. Pruneski said. “They bypass the need to get infected and allow people to get the immunity without having the actual disease.” Both the Pfizer and the Moderna vaccines are mRNA vaccines, while the Johnson and Johnson vaccine is a viral vector vaccine. In using these vaccines, Dr. Pruneski said, “If you can expose people to a part of the pathogen, then you can better protect them from the real thing.”
Risks, benefits, myths and facts were all topics of discussion. Dr. Pruneski noted that none of the vaccines make it into the nucleus of a cell, which is where DNA is stored, tackling the myth that vaccines can alter one’s DNA. “In fact, this is impossible to do and there is no evidence of a vaccine that can alter any existing DNA,” he said.
The risks of contracting COVID-19 include a 0.7% infection fatality rate, 5% hospitalization rate, and 30% chance of developing “long-haul” symptoms. COVID-19 is still relatively new, so scientists and health experts are still learning more about the potential for severe long-term side effects. A benefit of this is that the body can develop some immunity. For the COVID-19 vaccines, the risks are: mild short-term side effects, a 1-in-a-million chance of severe side effects, and knowledge yet to be learned about potential long-term side effects. The benefits of a vaccine are developing strong immunity (shown to be stronger than a natural infection), unlikely to spread the virus, and the reduction of restrictions of daily living brought on by the pandemic.
“The best vaccine to get is the one that is offered to you first and is available because they all offer high protection,” Dr. Pruneski said. He concluded the discussion by opening the floor up to students and faculty to ask their own questions about the virus and the vaccines. One question revolved around the different strains of the virus and the different infections from these strains.
“Vaccines are not as good at protecting against the new strains, but still show a lot of protection against these variants compared to not having the vaccine, even if it is not the full protection,” Dr. Pruneski said. “Variants will continue to arise by mutations and spread and we are at a point where we are racing to get the vaccine and beat those variants.”
-- by Amanda Overy, ’21